Self-reported outcome instruments or patient-reported outcome measures (PROMs) are gaining popularity.(1) Recently, there has been interest in using PROMs to aid management of individual patients – this is mainly due to the importance of monitoring the subjective effectiveness of received treatments, required in the current healthcare system to assess treatment quality.(1,2)
In Australia, WorkSafe (3) expects that all healthcare professionals who provide services to injured workers for longer than 4-6 weeks will use standardised or customised outcome measures to assist in the clinical justification of their services. (read more here)
The outcome of objective tests (e.g. orthopaedic tests performed by a clinician) does not necessarily correspond with subjective feelings of patients, whereas PROMs provide feedback on patients’ view of their complaints.(1)
PROMs can be used in clinical practice in various ways: they can be used as one-time screening questionnaires; alternatively, they can be administered serially to monitor patients’ progress and facilitate identification of problems.(2)
Worksafe and The Transport Accident Commission (TAC) note the need to evaluate the appropriateness of PROMs based on the individual patient’s needs and the clinician’s own professional expertise.(3,4) Furthermore, the TAC (4) state “It is often best to use more than one measure.” As such, clinicians need to select multiple PROMs in an attempt to cover the various domains of a patients’ presenting complaint(s).
Listed below are PROMs grouped according to their primary focus (3,4). As a general guideline, clinicians should select one PROM from each primary focus group, for each region (e.g. a patient presents with neck pain – the clinician would select one PROM for pain, another PROM for neck disability / function etc)
- Pain
- e.g. Quadruple Numerical Rating Scale (QNRS)
- Disability / Function
- e.g. Upper Extremity Functional Index (UEFI), Shoulder Pain and Disability Index (SPADI), Lower Extremity Functional Scale (LEFS) , Neck Disability Index (NDI) , Whiplash Disability Questionnaire (WDI), Quebec Back Pain Disability Scale (QBPDS)
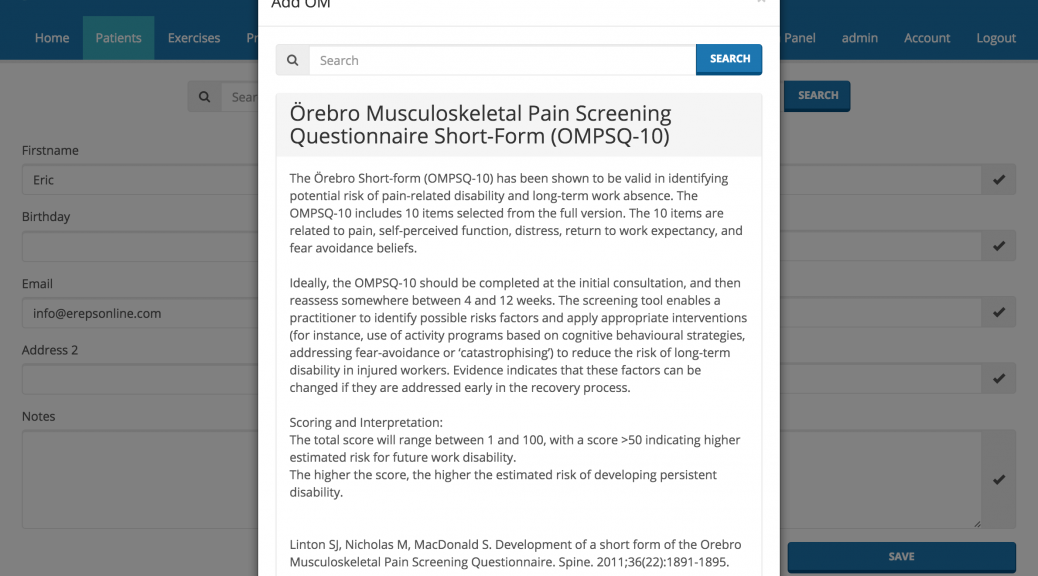
- Risk Identification / Predicting response to treatment (‘Yellow Flags’)
- Örebro Musculoskeletal Pain Screening Questionnaire Short-form (OMPSQ-10) (read more about the OMPSQ-10 here), Fear Avoidance Beliefs Questionnaire (FABQ) (read more about the FABQ here), Pain Self-Efficacy Questionnaire (PSEQ), Pain Catastrophizing Scale (PCS)
- General Health Status (Quality of Life)
- Short-Form 12 Health Survey (SF-12), RAND 36-Item Health Survey (SF-36)
Importantly, it has been shown that clinicians have incorrectly scored PROMs at a level that is of concern, and problematic!(5) A study by Matthey et al (5) suggest that clinicians adopt using scoring templates and a double adding-up procedure to reduce scoring errors… one of the great things about Erepsonline, is that you can save time and remove the human error when scoring outcome measures.
Easily administer, score and interpret outcome measures through Erepsonline – which may be used to assist your clinical practice. You must evaluate the appropriateness of the outcome measures based on the individual’s needs and your own professional expertise.
References
- Vuurberg G, Kluit L, van Dijk CN. The Cumberland Ankle Instability Tool (CAIT) in the Dutch population with and without complaints of ankle instability. Knee Surgery Sports Traumatol Arthrosc. 2018;26:882-891
- Snyder CF, Aaronson NK. Use of patient-reported outcomes in clinical practice. The Lancet. 2009;374(9687):369–70.
- WorkSafe. (n.d.). Outcome Measures. Retrieved from: http://www.worksafe.vic.gov.au/health-professionals/treating-injured-workers/outcome-measures
- TAC (Transport Accident Commission). Standard Outcome Measures. Retrieved from: http://www.tac.vic.gov.au/providers/working-with-tac-clients/clinical-resources/outcome-measures
-
Matthey S, Lee C, Črnčec R, Trapolini T. Errors in scoring the Edinburgh Postnatal Depression scale. Arch Womens Ment Health. 2013 Apr;16(2):117-22.